10 Hand Washing
On each square centimeter of your skin, there are about 1,500 bacteria. Some bacteria have been recently acquired from the environment and belong to a group called transient microbiota. But most belong to what is called the resident microbiota. These microorganisms (not only bacteria) that constantly live on and in our bodies. Transient microbiota are generally easily removed by washing. If you are handling material that is human- contaminated, the transient microbiota may include pathogens. You can pick up transient microbiota from your daily environment, such as doorknobs, faucets, tables, other people you interact with. Your resident microbiota plays a role in protecting you against any that may be pathogenic.
The resident microbiota of the skin live under the stratum corneum (the outermost layer of the skin), can be found on the surface, and in glands and follicles. Those microorganisms have learned to adapt to the many niches that they live in and tend to remain stable over time. (See pages 909-910, OpenStax, appended below). Different types of bacteria dominate the dry, moist, and sebum-rich regions of the skin. While hands are mostly dry, we also use them to touch sebaceous regions such as the face, neck and hair. The sebaceous secretions are antimicrobial. Staphylococcus, like S. epidermidis, are more typical of moist areas, but are also found on the hands. This microbiome aids in host defense by producing antimicrobial peptides that target the pathogens, preventing their establishment on the skin.
Even with the protection of resident microbiota, pathogens can cause infection. Microorganisms and their diseases are transmitted through direct and indirect contact. A simple but important approach in preventing the spread of disease is handwashing. The physicians by the names of Ignaz Semmelweis and Oliver Wendall Holmes are given the credit for the concept of disease prevention through hand washing. Semmelweis noticed a high death rate at child birth and puerperal infections when doctors did not wash their hands going from the autopsy room to delivery. He proposed the practice of washing with chlorinated lime solution. Holmes observed less infant deaths and puerperal infections when midwives carry out the deliveries compared to doctors. He proposed hand washing with calcium chloride. Both methods resulted in an increase of successful deliveries and decrease of infections.
In this experiment, you will be observing different types of hand washing and the effectiveness it has on removing both resident and transient microbiota from the skin. You will be comparing 4 scenarios: unwashed hands, vigorously washing with water, washing with soap (0.3% chloroxylenol), and washing with povidone iodine (13%) scrub.
The sebaceous secretions are an important consideration in this experiment. When we use a swab to transfer skin bacteria to a plate, we are also transferring antimicrobial sebaceous secretions. The bacteria are spread on a plate along with sebaceous secretions or other compounds such as found in hand moisturizer. These can inhibit microbial growth. Occasionally, we see larger number of colonies after hand-washing. This is part of the experiment and helps us understand the nature of the skin microbiome.
MATERIALS
Per pair of students should have:
Wax pencil
2 TSA plates (Trypticase Soy Agar)
4 Sterile swabs
1 Povidone iodine scrub brush
PROCEDURE OF HAND WASHING
- Label the bottom of each plate with student names and date. On each plate with a wax pencil, draw a line down the middle of the plate, dividing it half. Label as follows:
2. Designate one partner as the one being washed and the other as the sample collector. The student who is being washed will not touch anything: not the sink handles, the soap dispenser, the distilled water bottle, the TSA plates, anything. Simply do the scrubbing. The sample collector will be the one to touch all that was mentioned previously and be the one to take the samples off of the hand of the one being washed.
3. Unwashed hands: Place water from a distilled water bottle onto a hand, and spread between the two hands. This moistens the skin so that bacteria can be removed easily.
4. Then rub a sterile swab along the surface of the skin. After sample is collected, gently rub the swab along the surface of the TSA plate labeled “Unwashed”. (Note which side of the swab is used in the hand and use that side on the plate.)
5. Vigorously wash with water: Place hands and scrub together under running warm water for 60 seconds.
6. Then rub a sterile swab along the surface of the skin. After sample is collected, gently rub the swab along the surface of the TSA plate labeled “Water”.
7. Washing with soap: Place soap onto hands and then scrub together for 60 seconds. Rinse all soap off, to avoid including the effect traces of soap.
8. Then rub a sterile swab along the surface of the skin. After sample is collected, gently rub the swab along the surface of the TSA plate labeled “Soap”.
9. Wash with Iodine Scrub: Wet hands under running water. Then coat hands with sponge side of Povidone iodine scrub brush. Once well-coated, flip brush over and scrub with bristles for 60 seconds. Rinse all iodine off, completely.
10. Then rub a sterile swab along the surface of the skin. After sample is collected, gently rub the swab along the surface of the TSA plate labeled “Iodine”.
11. All swabs and scrub brushes can be placed in the regular trash can.
12. Once all samples are collected, the plates can be stored in your lab section’s rack at temperature. You will examine your results next lab.
REFERENCES
Brown, A. E. (2009). Benson’s Microbiological Applications: Laboratory Manual in General Microbiology. New York: McGraw Hill.
Chess, B. (2015). Laboratory Applications in Microbiology: A Case Study Approach. New York: McGraw Hill. Cogen, A., Nizet, V., & Gallo, R. (2008 Mar ). Skin microbiota: a source of disease or defence? British Journal of Dermatology, 442-455.
Cowan, M. K. (2015). Microbiology: A Systems Approach (4th edition). New York: McGraw Hill.
OpenStax. (2016, November 1). Microbiology. Retrieved from https://legacy.cnx.org/content/col12087/1.4
When and Why: Wash Your Hands . (2017, April 19). Retrieved from Minnesota Department of Health: http://www.health.state.mn.us/handhygiene/why/handsbacteria.html
From Openstax: p 908-910 Chapter 21: Skin and Eye Infections
21.1 Anatomy and Normal Microbiota of the Skin and Eyes
Learning Objectives
- Describe the major anatomical features of the skin and eyes
- Compare and contrast the microbiomes of various body sites, such as the hands, back, feet, andeyes
- Explain how microorganisms overcome defenses of skin and eyes in order to cause infection
- Describe general signs and symptoms of disease associated with infections of the skin and eyes
Human skin is an important part of the innate immune system. In addition to serving a wide range of other functions, the skin serves as an important barrier to microbial invasion. Not only is it a physical barrier to penetration of deeper tissues by potential pathogens, but it also provides an inhospitable environment for the growth of many pathogens. In this section, we will provide a brief overview of the anatomy and normal microbiota of the skin and eyes, along with general symptoms associated with skin and eye infections.
Layers of the Skin
Human skin is made up of several layers and sublayers. The two main layers are the epidermis and the dermis. These layers cover a third layer of tissue called the hypodermis, which consists of fibrous and adipose connective tissue (Figure 21.2).
The epidermis is the outermost layer of the skin, and it is relatively thin. The exterior surface of the epidermis, called the stratum corneum, primarily consists of dead skin cells. This layer of dead cells limits direct contact between the outside world and live cells. The stratum corneum is rich in keratin, a tough, fibrous protein that is also found in hair and nails. Keratin helps make the outer surface of the skin relatively tough and waterproof. It also helps to keep the surface of the skin dry, which reduces microbial growth. However, some microbes are still able to live on the surface of the skin, and some of these can be shed with dead skin cells in the process of desquamation, which is the shedding and peeling of skin that occurs as a normal process but that may be accelerated when infection is present.
Beneath the epidermis lies a thicker skin layer called the dermis. The dermis contains connective tissue and embedded structures such as blood vessels, nerves, and muscles. Structures called hair follicles (from which hair grows) are located within the dermis, even though much of their structure consists of epidermal tissue. The dermis also contains the two major types of glands found in human skin: sweat glands (tubular glands that produce sweat) and sebaceous glands (which are associated with hair follicles and produce sebum, a lipid-rich substance containing proteins and minerals).
Clinical Focus
Part1
Sam, a college freshman with a bad habit of oversleeping, nicked himself shaving in a rush to get to class on time. At the time, he didn’t think twice about it. But two days later, he noticed the cut was surrounded by a reddish area of skin that was warm to the touch. When the wound started oozing pus, he decided he had better stop by the university’s clinic. The doctor took a sample from the lesion and then cleaned the area.
- What type of microbe could be responsible for Sam’s infection?
Jump to the next Clinical Focus box.
Perspiration (sweat) provides some moisture to the epidermis, which can increase the potential for microbial growth. For this reason, more microbes are found on the regions of the skin that produce the most sweat, such as the skin of the underarms and groin. However, in addition to water, sweat also contains substances that inhibit microbial growth, such as salts, lysozyme, and antimicrobial peptides. Sebum also serves to protect the skin and reduce water loss. Although some of the lipids and fatty acids in sebum inhibit microbial growth, sebum contains compounds that provide nutrition for certain microbes.
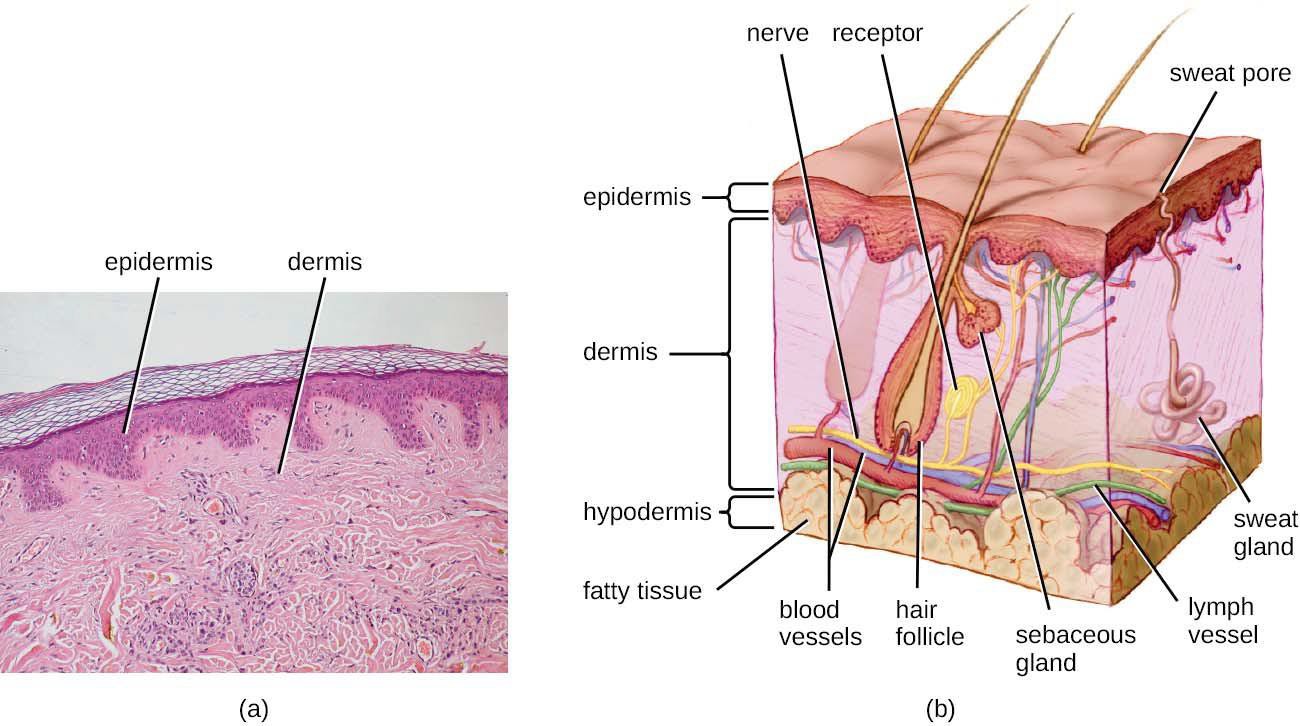
Figure 21.2 (a) A micrograph of a section through human skin shows the epidermis and dermis. (b) The major layers of human skin are the epidermis, dermis, and hypodermis. (credit b: modification of work by National Cancer Institute)

- How does desquamation help with preventing infections?
Normal Microbiota of the Skin
The skin is home to a wide variety of normal microbiota, consisting of commensal organisms that derive nutrition from skin cells and secretions such as sweat and sebum. The normal microbiota of skin tends to inhibit transient- microbe colonization by producing antimicrobial substances and outcompeting other microbes that land on the surface of the skin. This helps to protect the skin from pathogenic infection.
The skin’s properties differ from one region of the body to another, as does the composition of the skin’s microbiota. The availability of nutrients and moisture partly dictates which microorganisms will thrive in a particular region of the skin. Relatively moist skin, such as that of the nares (nostrils) and underarms, has a much different microbiota than the dryer skin on the arms, legs, hands, and top of the feet. Some areas of the skin have higher densities of sebaceous glands. These sebum-rich areas, which include the back, the folds at the side of the nose, and the back of the neck, harbor distinct microbial communities that are less diverse than those found on other parts of the body.
Different types of bacteria dominate the dry, moist, and sebum-rich regions of the skin. The most abundant microbes typically found in the dry and sebaceous regions are Betaproteobacteria and Propionibacteria, respectively. In the moist regions, Corynebacteriumand Staphylococcusare most commonly found (Figure 21.3). Viruses and fungi are also found on the skin, with Malasseziabeing the most common type of fungus found as part of the normal microbiota. The role and populations of viruses in the microbiota, known as viromes, are still not well understood, and there are limitations to the techniques used to identify them. However, Circoviridae, Papillomaviridae, and Polyomaviridae appear to be the most common residents in the healthy skin virome.[1][2][3]
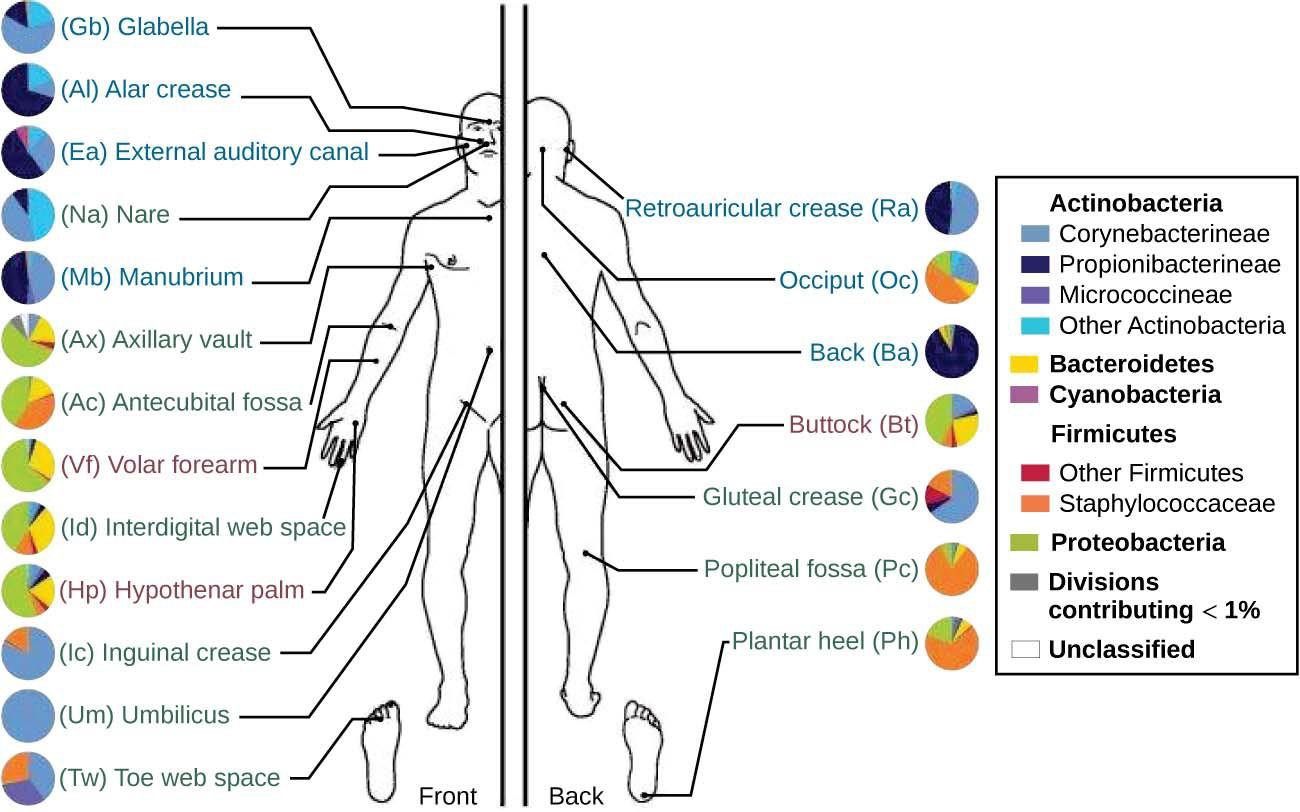
Figure 21.3 The normal microbiota varies on different regions of the skin, especially in dry versus moist areas. The figure shows the major organisms commonly found in different locations of a healthy individual’s skin and external mucosa. Note that there is significant variation among individuals. (credit: modification of work by National Human Genome Research Institute)
REFERENCES
Belkaid, Y., and J.A. Segre. “Dialogue Between Skin Microbiota and Immunity,” Science 346 (2014) 6212:954- 959.
Foulongne, Vincent, et al. “Human Skin Microbiota: High Diversity of DNA Viruses Identified on the Human Skin by High Throughput Sequencing.” PLoS ONE (2012) 7(6): e38499. doi: 10.1371/journal.pone.0038499.
Robinson, C.M., and J.K. Pfeiffer. “Viruses and the Microbiota.” Annual Review of Virology (2014) 1:55-59. doi: 10.1146/annurev- virology-031413-085550.
This OpenStax book is available for free at http://cnx.org/content/col12087/1.4
