4 Cardiovascular System
Learning Objectives
- Identify the functions of the cardiovascular system.
- Distinguish the structural and functional differences between arteries, veins, and capillaries.
- Identify the 4 heart chambers, 4 heart valves, and large blood vessels that connect to the heart.
- Outline the path of blood flow through the heart.
- Compare the features of a human heart model with those of a sheep heart.
- Describe the major events of the cardiac cycle.
- Correlate the sounds of the heartbeat during the cardiac cycle with the heart valves.
- Measure blood pressure and understand how blood pressure can change between resting state and after exercise.
- Identify the components of the cardiac conduction system.
- Identify the waves and segments of an electrocardiogram and state what they represent.
CARDIOVASCULAR SYSTEM
The cardiovascular system consists of the heart and blood vessels. The heart is considered a double pump as the right side pumps oxygen-poor blood through the pulmonary circuit (to the lungs) and the left side pumps oxygen-rich blood through the systemic circuit (to the rest of the body) (Figure 4.1). These circuits include the blood vessels called arteries, veins, and capillaries. Arteries carry blood away from the heart. Veins carry blood to the heart. Capillaries connect the arteries and veins as capillary networks. Capillaries are the smallest vessels with walls that are a single-cell layer thick, to allow for gas exchange, transport of nutrients, and removal of wastes. Arteries and veins are larger vessels, with walls that have three layers. The middle smooth muscle layer of artery walls is thicker than that of the veins so they can withstand the high blood pressure generated by the pumping of the heart as the arteries carry blood away from the heart. Another difference between arteries and veins is that veins have valves whereas arteries do not. These vein valves ensure one-way blood flow to the heart and prevent backflow as veins conduct blood from all over the body back to the heart (Figure 4.2).
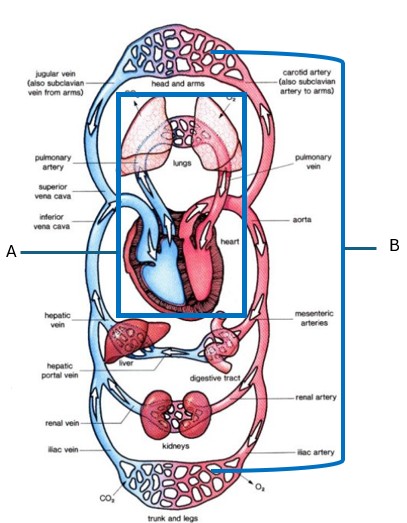
Figure 4.1 Pulmonary and systemic circuits of the cardiovascular system.
Note to students: Write all data and answers to questions on the Lab Report provided.
Activity 1: Identify the two circuits of the cardiovascular system.
Label each circuit of the cardiovascular in Figure 4.1 by using the text and recording your answers on the Lab Report.
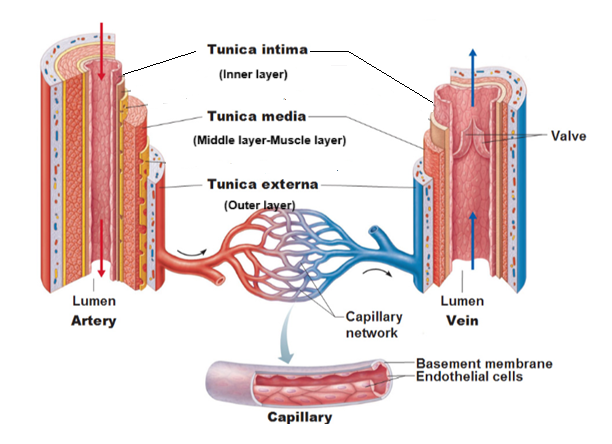
Figure 4.2: Comparison of the structure of artery, vein, and capillary.
Activity 2: Distinguish structural differences of the types of blood vessels.
Record your answers to the following questions on the Lab Report.
- Which type of blood vessel has walls that are only one cell thick: artery, vein, or capillary?
- What process occurs due to the vessel walls being only one cell thick?
- What is the scientific name of the outer layer of an artery and vein?
- What is the scientific name of the middle layer of an artery and vein?
- What is the scientific name of the inner layer of an artery and vein?
- Which layer of an artery and vein is made up of muscle tissue?
- Which type of blood vessel has a thicker middle muscle layer: artery or vein?
- Which type of blood vessel has valves: artery or vein?
The cardiovascular system has three basic functions: transportation, protection, and maintaining homeostasis. It transports oxygen, nutrients, hormones, and electrolytes to cells throughout the body. It also transports waste products, such as carbon dioxide, nitrogenous wastes, and other metabolic waste products, from the cells to the lungs and kidneys to be removed from the body. By carrying various white blood cells and antibodies, the cardiovascular system helps protect the body from infections and diseases. It also prevents excessive blood loss in case of injuries by carrying platelets and blood clotting proteins. Lastly, the cardiovascular system helps maintain homeostasis by regulating body temperature, blood pressure, pH, water and electrolyte balances.
ANATOMY OF THE HEART
The heart has four muscular chambers. The upper chambers are the left and right atria (singular: atrium). They have thin walls that are elastic due to containing significant amount of elastic fibers which allow them to stretch and recoil as they fill and empty with blood. The atria are divided by the interatrial septum. The lower chambers are the left and right ventricles. They have thick muscular walls where the wall of the left ventricle is thicker than that of right ventricle. The left ventricle wall is thicker so that it can pump oxygen-rich blood through the systemic circuit, but the thinner walled right ventricle only has to pump oxygen-poor blood through the pulmonary circuit (a smaller circuit). The ventricles are divided by the interventricular septum.
EXTERNAL ANATOMY
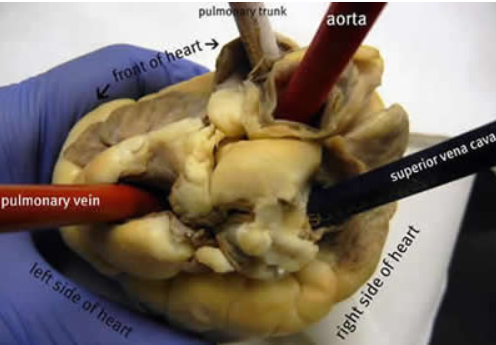
Figure 4.3 illustrates the external anatomy of the heart, showing the two large veins, superior vena cava and inferior vena cava, that carry oxygen-poor blood to the right atrium of the heart. The superior vena cava returns blood from the head, neck, chest, and upper limbs whereas the inferior vena cava returns blood from the abdomen, pelvis, and lower limbs.
Inferior to (below) the right atrium is the right ventricle. The large artery that is attached to the top of the right ventricle is the pulmonary trunk, which divides into the right and left pulmonary arteries. They carry oxygen-poor blood to the lungs where it is oxygenated.
From the lungs, the left and right pulmonary veins carry oxygen-rich blood back to the left atrium of the heart. Inferior to (below) the left atrium is the left ventricle. The large artery attached to the top of the left ventricle is the aorta. It bends to form the aortic arch. It carries oxygen-rich blood all over the body through the systemic circuit.
Branching from the aorta, coronary arteries run along the exterior surface of the heart. These arteries provide the heart muscle itself with oxygen-rich blood. The cardiac veins carry oxygen-poor blood from the heart muscle itself, draining into the coronary sinus on the posterior side of the heart into the right atrium.
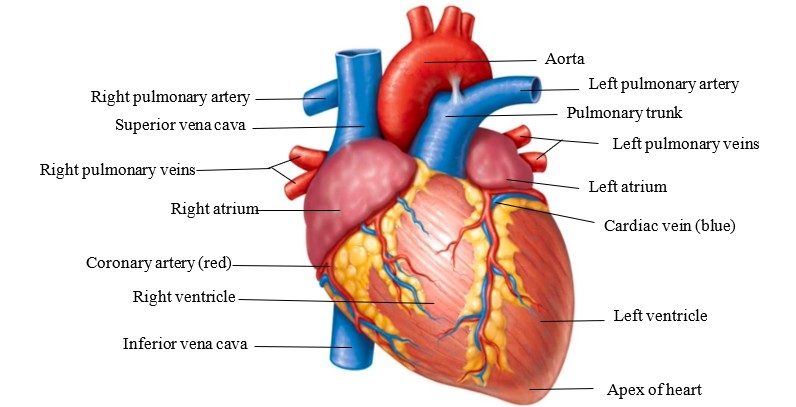
Figure 4.3 External anatomy of the heart. © John Wiley & Sons, Inc
INTERNAL ANATOMY
In the coronal section of the heart shown in Figure 4.4a, the front of the heart is separated from the back of the heart, and the internal anatomy of the heart can be observed. The four chambers (right atrium, right ventricle, left atrium, and left ventricle) are visible. The heart has two sets of valves. One set is called atrioventricular (AV) valves as they are located between the atria and the ventricles. The right atrioventricular valve is also called the tricuspid valve and is between the right atrium and right ventricle. The left atrioventricular valve is also called the bicuspid or mitral valve and is between the left atrium and left ventricle. Attached to both AV valves are chordae tendineae, fibrous chords connecting the AV valves to the papillary muscles, which are extensions of the inner walls of the ventricle muscle. As the ventricles contract, the papillary muscles pull on the chordae tendineae to ensure that the valves are tightly shut. This prevents backflow of the blood from the ventricles into the atria.
The other set of heart valves are the semilunar valves, so named because of their moon-like shape. These are found in the large arteries that emerge from the ventricles. The pulmonary semilunar valve is located in the base of the pulmonary trunk. The aortic semilunar valve is in the base of the aorta. These valves prevent the backflow of blood from the large arteries into the ventricles.
Figure 4.4b illustrates the path of blood through the heart.
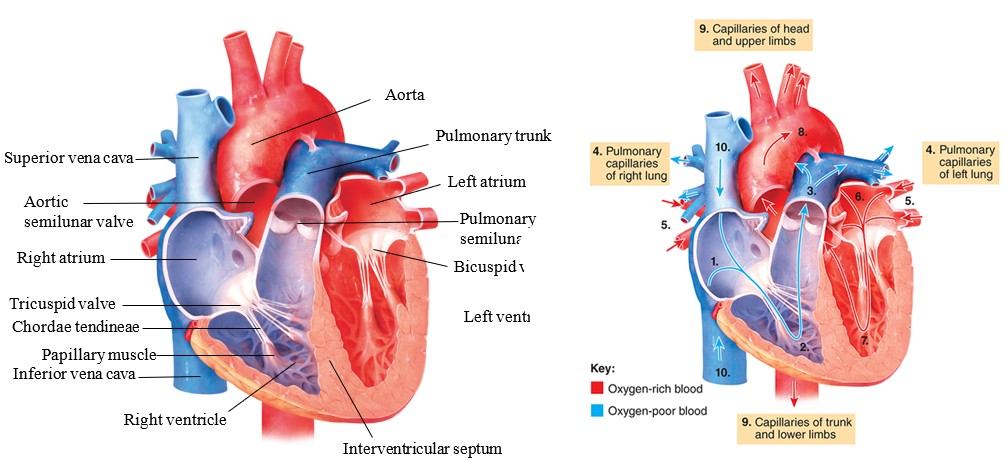
Figure 4.4 (a) Internal anatomy of the heart; (b) Path of blood flow through the heart © John Wiley & Sons, Inc
Activity 3: Trace the path of blood through the heart
Referencing the text and Figure 4.4(b), beginning with the right atrium, trace the path of blood flow through the heart by identifying the parts of the heart associated with the labeled numbers on the image of the heart.
Activity 4: Dissection of the Sheep Heart
Use gloves and safety glasses for this activity
- Obtain one sheep heart per lab bench along with one dissecting tray, scalpel, and dissecting probe.
- Identify the following structures of the external anatomy of the sheep heart: right atrium, right ventricle, left atrium, left ventricle, coronary arteries, and adipose (fat) tissue. Record answers on the Lab Report.
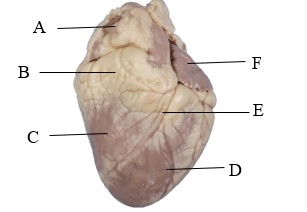
- Identify the following large blood vessels: superior and inferior vena cava, pulmonary trunk, and aorta. Insert a dissecting probe through the vessels to compare the thickness of walls.
- Place the superior part of the heart (top part with the large blood vessels attached) on the dissecting tray so that the apex of the heart is facing upwards.
- Using a scalpel, cut into the apex of the heart, slicing the sheep heart in half along the coronal plane.

- Identify the following structures of internal anatomy of the sheep heart in Figure 4.5: the 4 chambers of the heart, interventricular septum, 2 AV valves, and aorta. Compare the thickness of the left and right ventricle walls.
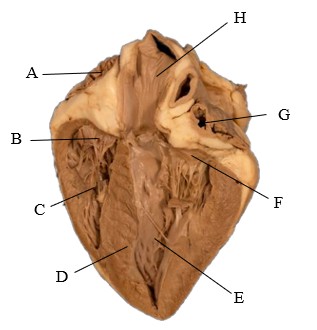
Figure 4.5 Internal anatomy of a sheep heart. - After dissection is completed, discard the sheep heart in your section’s designated bucket near the instructor table.
- Wash all dissecting tools & tray. Return all supplies to the proper location.
CARDIAC CYCLE AND BLOOD PRESSURE
The cardiac cycle is the series of events that occur in the heart during one heartbeat. It can be divided into two phases: systole (contraction) and diastole (relaxation) of the heart’s chambers. The atria and ventricles alternately contract and relax in one cardiac cycle. The walls of both atria contract simultaneously while the ventricular walls relax. Then both atrial walls relax while the ventricular walls contract. This forces the blood from areas of higher pressure to areas of lower pressure. When a chamber of the heart contracts, blood pressure within it increases.
HEART SOUNDS
During the cardiac cycle, the heart valves are opening and closing. The atrioventricular valves are open and the semilunar valves are closed during atrial systole. Then the atrioventricular valves are closed and the semilunar valves are opened during ventricular systole. Closing of the heart valves produces vibrations in the heart tissue creating the sounds associated with the heartbeat: lub-dub. The lub sound is the first sound heard when listening to the heartbeat with a stethoscope. It is caused by the atrioventricular valves closing. The dub sound is the second sound and is caused by the semilunar valves closing.
Activity 5: Listening to the Heartbeat at Rest
In order to listen to the heartbeat, work in pairs and designate one person as the subject and the other as the experimenter.
- Obtain a stethoscope and alcohol swab. Clean the earpieces and diaphragm of the stethoscope with the alcohol swab.
- Place the earpieces into the experimenter’s ears. Then the experimenter will place the diaphragm of the stethoscope on the left side of the subject’s chest between the fourth and fifth rib. This is where the apex of the heart is located.

- Listen quietly. Which sound is louder: lub/1st sound or dub/2nd sound?
- Move the diaphragm of the stethoscope to the subject’s left side of their chest but now between the second and third rib, just left of the sternum.

- Listen quietly. Which sound is louder: lub/1st sound or dub/2nd sound?
- Now students switch roles and repeat Steps 1-5.
- Record answers to questions on the Lab Report.
BLOOD PRESSURE
Each time the heart ventricles contract there is an increase in the force of the blood leaving the heart and pressing against the inner walls of the arteries. It is possible to measure the force of the blood flow, which is called blood pressure. Blood pressure reaches a maximum during ventricular contraction (systole) and then drops to its lowest level while the ventricles relax (diastole). The normal blood pressure at rest for an adult, measured in millimeters of mercury (mm Hg) is 120/80 (systole/diastole).
Activity 6: Measuring Blood Pressure with a sphygmomanometer
In order to measure blood pressure, work in pairs and designate one person as the subject and the other as the experimenter.
Blood Pressure at Rest
- Have the subject sit in a lab chair and remain relaxed for a minute or two, taking deep breaths.
 The experimenter will place the digital sphygmomanometer cuff onto the subject’s left or right upper arm with the tubing running along the inner elbow.
The experimenter will place the digital sphygmomanometer cuff onto the subject’s left or right upper arm with the tubing running along the inner elbow.- Experimenter will turn on the sphygmomanometer, closing the valve on the pump bulb by rotating the knob. After 3 beeps, pump the bulb until the device reads 160. Subject will remain still.
- When the experimenter stops pumping, the numbers on the display will decrease as the cuff naturally deflates. You will also see a flashing heart icon on the display.
- The device should beep once and then display systolic pressure, diastolic pressure, and heart rate. Record the blood pressure reading in Table 4.1 on the Lab Report.
- After the measurement is displayed, press the button under the bulb to release the air in the cuff .
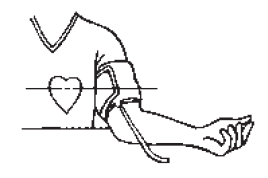
Blood Pressure after Exercise
- Experimenter will close the valve on the pump bulb by rotating the knob.
- While wearing the sphygmomanometer, subject will run in place for 1 minute.
- Immediately after the exercise the experimenter will pump the bulb until the device reads 160.
- The numbers on the display will decrease as the cuff naturally deflates and a flashing heart icon will display.
- When the device beeps once, record the blood pressure reading in Table 4.1 on the Lab Report.
- After the measurement is displayed, press the button under the bulb to release the rest of the pressure.
CARDIAC CONDUCTION SYSTEM
The heartbeat is a rhythmic pumping action that is controlled by the cardiac conduction system. The cardiac conduction system (Figure 4.6) is a network of specialized cells that generate and transmit electrical impulses through the heart. The heartbeat is initiated by autorhythmic cardiac cells called the sinoatrial (SA) node, also known as the natural pacemaker, that is located in the right atrium. The SA node triggers the atria to contract by sending an electrical impulse through the walls of the atria to the atrioventricular (AV) node. The AV node is in the interatrial septum. It delays the electrical impulse to give the atria time to pump blood into the ventricles. The impulse then travels to the atrioventricular (AV) bundle, down through the interventricular septum via the left and right bundle branches. The Purkinje fibers transmit the impulse through the walls of the ventricles, causing ventricular contraction.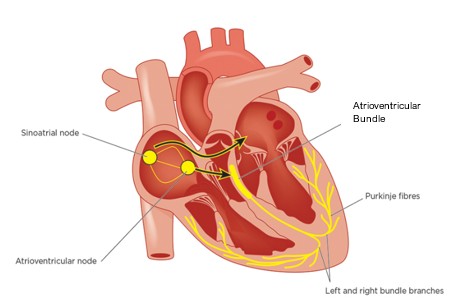
Figure 4.6 Cardiac conduction system
The electrical activity of the cardiac cycle can be visualized using electrocardiography (ECG) (Figure 4.7). The ECG is a repeating pattern or graph of peaks and valleys that represent cardiac electrical activity. The first wave of an electrocardiogram is the P wave, which represents atrial depolarization, or the spreading of the electrical signal of the SA node through the atrial walls. The second wave is the QRS wave, which represents ventricular depolarization, or the passage of the electrical signals from the AV node through AV bundle and bundle branches of the ventricular walls. The third wave is the T wave, which is caused by the recovery of the ventricles, or ventricular repolarization. The shapes and spacings of these waves enable clinical diagnosis of cardiovascular disease.
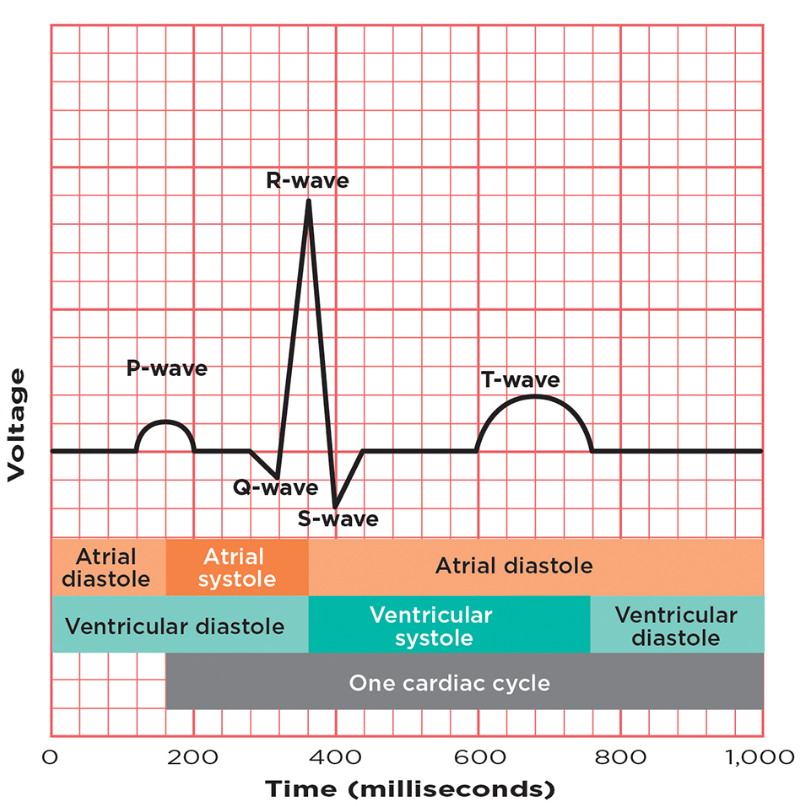
Figure 4.7 A normal electrocardiogram indicates that the heart is functioning properly. The P wave indicates that the atria are about to contract; the QRS wave indicates that the ventricles are about to contract; and the T wave indicates that the ventricles are recovering from contraction.
Activity 7: Measuring Heart Activity by Using Electrocardiography (ECG)
Usually when performing electrocardiography, the subject has 12 electrodes attached to their body on the limbs and chest, but we will only be using 4 electrodes (in one position on each limb) to record one lead, specifically Lead II. Lead II measures the electrical impulse differences between the right arm and left leg during cardiac activity. The display screen will show Leads I, II, and III, but only Lead II will print.
You will be working in groups of up to 4 individuals using one ECG machine per lab bench. You can take turns being the subject or experimenter so that each student gets a turn in both roles. The subject should remove any jewelry from their wrists and ankles.
- Clean the inner side of the wrists and ankles with an alcohol swab.
- Apply one self-adhesive electrode to each wrist and ankle.
- Attach the corresponding lead to each electrode using the clamps:
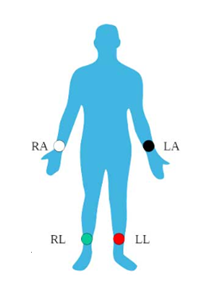
LL (Red) = Left Leg
RL (Green) = Right Leg
LA (Black) = Left Arm
RA (White) = Right arm - The subject will sit still and relaxed in a lab chair. Make sure not to move your arms or legs.
- If the instrument is off, the experimenter may have to press the Power Button. Then press the F2 (marked by blue tape) until Leads I, II, and III are shown on the screen.
- Next press the Rhythm button (marked by green tape). Let the ECG run until at least 2 pages print.
- Press the Stop button (marked by pink tape).
- After the ECG is complete, remove the electrodes from the subject’s wrists and ankles and dispose of them in the regular garbage can. The subject may use soap and water to remove any remaining adhesive.
- If time allows, each student can get a turn being experimenter or subject. Repeat Steps 1-8.
- Cut and tape an electrocardiogram on the Lab Report. Answer any questions.
Activity 8: Lab Review
On the Lab Report, answer the questions in the Lab Review section.
Link to Lab Report: Lab 4 Cardiovascular System Lab Report
REFERENCES
Antranik Training Program. (2024, December 11). Blood vessels. https://antranik.org/blood-vessels/
Biology Corner. (n.d.). Sheep Heart Dissection-A Step by Step Guide. https://www.biologycorner.com/worksheets/heart_dissection.html
Darling, David. (2016). circulatory system. https://www.daviddarling.info/encyclopedia/C/circulatory_system.html
Dias, G. R. (2018, March 9). A General Study on Stethoscopes. https://www.linkedin.com/pulse/general-study-stethoscopes-gaston-ravin-dias/
Jarvis, S., & Contributor, N. (2021, May 17). Electrocardiogram 1: purpose, physiology and practicalities. Nursing Times. https://www.nursingtimes.net/cardiovascular/electrocardiogram-1-purpose-physiology-and-practicalities-17-05-2021/
Mader, Sylvia S. (2023). Laboratory Manual for Human Biology. 17th edition. McGraw-Hill.
Tenor. (2016, November 2). Heartbeat Conduction GIF – Heartbeat Conduction Heart – Discover & Share GIFs. https://tenor.com/view/heartbeat-conduction-heart-blood-cardiology-gif-7044974?utm_source=share-button&utm_medium=Social&utm_content=pinterest
Tortora, Gerard J. and Bryan H. Derrickson. (2016). Principles of Anatomy and Physiology, 15th edition. John Wiley and Sons.
Welsh, Charles and Cynthia Prentice-Craver. (2023). Hole’s Essentials of Human Anatomy and Physiology. 15th edition. McGraw-Hill

